Provider volumes for medically necessary and preventive care visits dropped dramatically at the start of the COVID-19 pandemic. Volumes for medically necessary visits have largely rebounded because of the relaxed telehealth and in-person visit guidelines, and providers have an opportunity to regrow preventive visit volumes as well.
In response to the COVID-19 Public Health Emergency (PHE) issued on March 1, 2020, the Centers for Medicare & Medicaid Services (CMS) expanded access to telehealth services so that Medicare beneficiaries could continue to receive services from their providers without traveling to provider offices or health care facilities.

The expanded telehealth services included evaluation and management visits, mental health counseling, and preventive services. Medicare’s Annual Wellness Visit (AWV) is a preventive service and therefore may be performed via telehealth. The Annual Wellness Visit is a yearly visit that Medicare Part B covers for most enrollees. It is an opportunity for providers to focus on prevention, review health history, reconcile medications, and identify any immunizations or preventive screenings that might be needed. The Annual Wellness Visit is not a full head-to-toe physical exam. It offers the opportunity for providers to ensure that a beneficiary’s risks, if still current, are screened, documented, and evaluated to create the beneficiary’s personalized prevention plan.
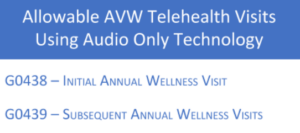
Prior to the Public Health Emergency, the Annual Wellness Visit was on the CMS list of covered telehealth services that required the use of real-time audio and video. Beginning on March 1, 2020, CMS permitted certain telehealth services to be rendered using audio-only communications technology. The initial and subsequent Annual Wellness Visit is now listed as a service that can be performed using a telephone or audio-only device, and the visit itself can be performed at the beneficiary’s home.
Whether an initial or subsequent Annual Wellness Visit is being performed, CMS requires the provider to collect and document the beneficiary’s height, weight, body mass index (BMI), blood pressure, and any other routine measurements deemed appropriate based on medical and clinical history. CMS issued COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing document, which states that if Annual Wellness Visits are performed when beneficiaries are at home, they may self-report their vitals provided they have the proper equipment needed to self-report. If a patient self-reports, the measurements should be recorded in the medical record as reported by the patient. If the visit meets all the other Annual Wellness Visit requirements, it can be billed as an PHE. During the Public Health Emergency, the Place of Service (POS) should be billed to the address where the service would have taken place in the absence of the emergency (most likely POS 11), and the appropriate modifier should be added.
As the Public Health Emergency continues, telehealth services are a good alternative for the traditional model of care for both medically necessary and preventive care. Performing Annual Wellness Visits via telehealth provides the opportunity to increase patient engagement and satisfaction, address any gaps in care, lower the cost of care delivery, address pay-for-performance measures, and drive business growth, quality scores, and revenue.
Keeping abreast of changes during the Public Health Emergency is vital to the growth and sustainability of your organization. For additional information on establishing an Annual Wellness Visit telehealth service and other sustainable solutions that fit your organization’s needs, please contact Vickie Bridge at vbridge@pinnnaclehca.com.